Applications
Cell Therapy
While the research industry is evolving fast, various cell types will be developed into treatments as novel cell therapeutics and studied for future applications. Human mesenchymal stem cells (MSCs) are widely used because of their interesting and promising results. These MSCs are multipotent cells that are capable of self-renewal and differentiation which can be isolated from bone marrow, umbilical cord, adipose tissues and others.
Cellular therapy (CT) background
Cellular Therapy (CT) is the transplantation of human cells to regenerate, replace, and repair damaged cells and tissues. Cell therapy practices date back to the 19th century and continue to expand on investigational and investment grounds. Cell therapy refers to the transfer of autologous or allogeneic cellular material into a patient for medical purposes. The year 1889 witnessed the first practices of cell therapy by Charles-Édouard Brown-Séquard—pioneer in hormone therapy at the time—who attempted to suppress the effects of aging using injections of animal testicle extracts. Today, cell therapy continues to evolve with ongoing investigations for clinical safety and efficacy, and with a global market size estimated to expand from USD 9.5 billion in 2021 to USD 23.0 billion in 2028.
Cell therapy includes stem cell- and non–stem cell-based, unicellular, and multicellular therapies, with different immunophenotypic profiles, isolation techniques, mechanisms of action, and regulatory levels. With new state-of-the-art technologies, innovative products, and limitless discoveries, a diverse number of cells may be used as a treatment for a wide variety of diseases and medical conditions- infectious, degenerative, autoimmune, cancer, and many more. Cellular Therapy started to play a vital role in the practice of medicine. Its technologies overlap with those of gene therapy, cancer vaccines, drug delivery, tissue engineering and regenerative medicine.

The aim of cellular therapy is to prevent and treat human diseases via administration of cells that have been treated, altered, or engineered ex vivo. Main applications include treatment of cardiac diseases, diabetes mellitus, bones and joints disease, genetic disorders, skin/soft tissue wounds, and cancer.
Stem Cell for Cellular Therapy
Stem cells can be found in an organism in embryos and adult cells; they are a type of unspecialized, self-renewable cells prepped to differentiate into any cell type and/or as many cell types. What dictates how many cell types stem cells can differentiate into is their developmental potency. Developmental potency represents a differentiation continuum starting with totipotency (i.e., highest differentiation potential; e.g., zygote) and dwindling to pluripotency (e.g., embryonic stem cells), multipotency (e.g., hematopoietic stem cells), oligopotent (e.g., myeloid stem cells), and unipotency (i.e., least differentiation potential; e.g., dermatophytes)
Stem cells are the ideal cells to be used for cell therapy because of their two main properties: ability to replicate for long periods of time and to develop into different cell types. There are 3 major types of stem cells:
- embryonic stem cells,
- adult stem cells, and
- induced pluripotent stem cells (iPSCs);
The first two are naturally found, while iPSCs are produced in the laboratory.
Embryonic stem cells
Embryonic stem cells are derived from preimplantation embryos, which are capable of indefinite and undifferentiated proliferation. B Primate ES cells retain their ability to distinguish between trophoblast and embryonic endoderm, mesoderm, and ectoderm derivatives. Since these cells have the differentiation capacity to almost all cells or tissue, they have a good advantage to cure several diseases, including diabetes mellitus, Alzheimer’s, anemia and spinal cord injuries.
Embryonic stem cells have an unlimited capacity for self-renewal as well as the potential to differentiate into every cell type in the body. These characteristics make hESC an extremely attractive cell source for regenerative medicine; derivatives may be used to repair damaged tissue or replace specific cells lost due to disease. Numerous hESC-based therapies have shown promise in animal models, and several of them are now in human clinical trials.
Human embryonic stem cells undifferentiated cells obtained from a 5-day pre-implantation embryo. Embryonic stem cells are pluripotent, whereby they can give rise to ALL kinds of cells in the human body.

Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells (iPSCs or iPS cells), are a type of pluripotent stem cell derived from adult somatic cells that have been genetically reprogrammed to an embryonic stem (ES) cell-like state through the forced expression of genes and factors important for maintaining the defining properties of ES cells. They are genetically engineered adult cells, programmed to behave like pluripotent embryonic stem cells.
The method of reprogramming somatic cells into iPS cells was first demonstrated that genomic integration and high expression of four factors, by virus, can reprogram fibroblast cells into iPS cells. iPS cells can be generated from fibroblasts by viral integration without c-Myc. Although these iPS cells showed reduced tumorigenicity in chimeras and progeny animal models, the reprogramming process is much slower, and efficiency is substantially reduced.
Various growth factors and chemical compounds have recently been found to improve the induction efficiency of iPS cells. Shi et al., demonstrated that small molecules, able to compensate for Sox2, could successfully reprogram mouse embryonic fibroblasts (MEF) into iPS cells.
Strenuous efforts are being made to improve the reprogramming efficiency and to establish iPS cells with either substantially fewer or no genetic alterations. Besides reprogramming vectors and factors, the reprogramming efficiency is also affected by the origin of iPS cells.
Adult stem cells
Adult stem cells, also known as somatic stem cells, are undifferentiated cells found in different areas of the body. They differ from embryonic stem cells as they are multipotent, whereby they can only develop into specific types of cells. Adult stem cells include the following:
Hematopoietic stem cells
Hematopoietic stem cells (HSCs) are adult stem cells that can develop into all types of blood cells, including myeloid-lineage and lymphoid-lineage cells. HSCs can be found in several organs, such as peripheral blood (PB), bone marrow (BM), and umbilical cord blood (UCB). All blood cell lineages are produced via functional maturation of a rare population of multipotent HSCs that can proliferate by self-renewal and differentiation.
Hematopoietic stem cell (HSC) therapy involves the intravenous infusion of autologous or allogeneic stem cells to reconstruct a functional hematopoietic system in patients with blood disorders. HSC therapy is used to treat the following disorders, such as leukemia, including acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), non-Hodgkin lymphoma (NHL), chronic myeloid leukemia (CML), chronic lymphocytic leukemia (CLL), myeloproliferative disorders, multiple myeloma (MM), lymphoma and Hodgkin disease (HD). Autologous HSC therapy has been used as a therapeutic option among patients with both multiple myeloma (MM) and lymphoma. Meanwhile, allogeneic HSC therapy is more popular for many types of diseases, including malignant and non-malignant disorders including leukemia, including AML, ALL, chronic myeloid leukemia (CML), and chronic lymphocytic leukemia (CLL). HSC therapy has been improved and improved techniques, such as gene transfer with HSC therapy, could be used to treat a variety of diseases.
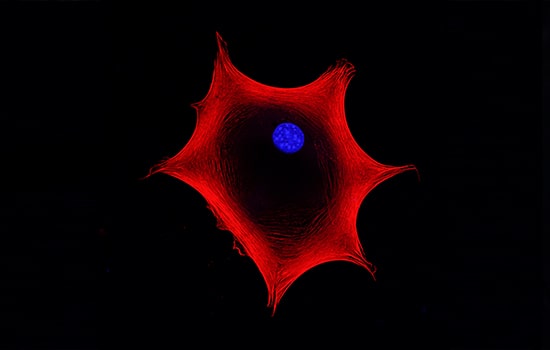
Mesenchymal stem cells
Mesenchymal stem cells (MSCs), also referred to as mesenchymal stromal cells, are adult stem cells capable of self-renewal and multilineage differentiation. They were originally found in the bone marrow, but they were later identified in other tissues including adipose tissue, muscle, peripheral blood, hair follicles, teeth, placenta and umbilical cord. Although MSCs may exhibit different characteristics depending on their tissue of origin, they must meet the three minimal criteria defined by the International Society for Cellular Therapy (ISCT):
- First, MSCs must show plastic-adherence when grown in vitro.
- Second, MSCs must express the surface antigens CD73, CD90, and CD105 while lacking expression of CD45, CD34, CD14 or CD11b, CD79α or CD19 and HLA-DR.
- Third, MSCs must differentiate into mesodermal cell types (i.e., adipocytes, chondrocytes, and osteoblasts) when cultured under specific conditions. In addition to mesodermal lineage.
Mesenchymal stem cells (MSCs) are capable of differentiating into cells of non-mesodermal origin (ectodermal and endodermal lineages), such as neuronal cells, cardiomyocytes, hepatocytes or epithelial cells. This plasticity of MSCs confers benefits in tissue regeneration.
Mesenchymal stem cells (MSCs) also possess the capacity to migrate to injured sites in response to environmental signals and promote tissue regeneration mediated by the release of paracrine factors with pleiotropic effects. Through interaction with the host niche, MSCs are able to inhibit the immune system, promote cell survival, or induce angiogenesis among other pleiotropic activities. Of these, the immunosuppressive role of MSCs is particularly interesting for clinical use since it confers resistance to rejection by the host immune system after transplantation. Furthermore, MSCs can be obtained from easily accessible sources by minimally invasive methods (peripheral blood, adipose tissue) and can be rapidly expanded in large-scale for clinical use. This allows the production of a patient-specific medicinal product (i.e., autologous medicinal product) within a therapeutic time window. In addition, the possibility of obtaining MSCs from adult tissue circumvents the ethical issues associated with the use of embryonic sources. All these advantages of MSCs make this cell type a powerful tool for clinical application in regenerative medicine.
Neural stem cells
Neural stem cells (NSCs) differentiate into brain cells including nerve cells (neurons), astrocytes, and oligodendrocytes. In adults, a small number of NSCs remain and are mostly quiescent; however, ample evidence supports their important roles in plasticity, aging, disease, and regeneration of the nervous system. Because NSCs are regulated by both intrinsic genetic and epigenetic programs and extrinsic stimuli transduced through the stem cell niche, dysregulation of NSCs due to either genetic causes or environmental impacts may lead to disease.

Skin stem cells
Skin stem cells give rise to different cells, depending on where they are found; those found at the base of the hair follicle differentiate into the epidermis or the hair follicle and those found in the basal layer of the epidermis result in keratinocytes.
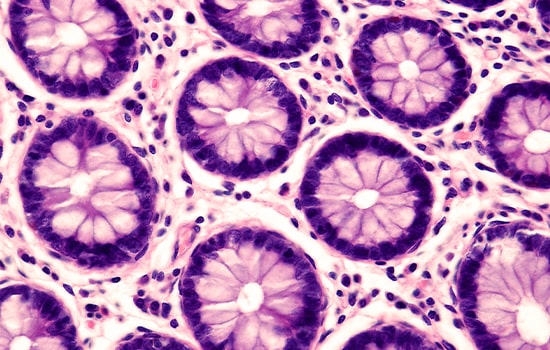
Epithelial stem cells
Epithelial stem cells result in absorptive cells, goblet cells, paneth cells, and enteroendocrine cells and can be found in the lining of the digestive tract.
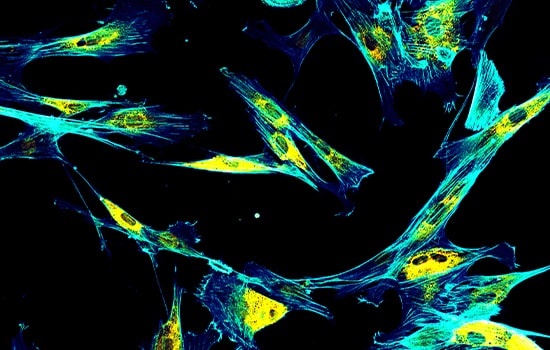
Esco Healthcare offers its Tide Motion platform that is ideal in cultivating billions of anchorage dependent cells like hMSCs. hMSCs can expand easily with bioreactor as the adherent cell culture for cell therapy in regenerative medicine. Several cell therapies in regenerative medicine have become either established practices or commercially available with FDA approval, such as keratinocyte- and/or fibroblast-derived skin substitutes for treatment of diabetic foot ulcers or burns, keratinocyte and fibroblast-containing scaffold products for treatment of surgically created vascular wound beds in the oral cavity, fibroblast intradermal injections for improvement of appearance of nasolabial fold wrinkles, and chondrocyte-containing scaffold implants for treatment of knee cartilage defects.
Sources
- Abed El-Hakim El-Kadiry, Moutih Rafei, and Riam Shammaa. 2021. Cell Therapy: Types, Regulation, and Clinical Benefits. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8645794/. Published online 2021 Nov 22. doi: 10.3389/fmed.2021.756029. 2021; 8: 756029.
- Worku MG. 2021. Pluripotent and Multipotent Stem Cells and Current Therapeutic Applications: Review. 12 April 2021 Volume 2021:14 Pages 3—7. DOI https://doi.org/10.2147/SCCAA.S304887
- Lei Ye, Cory Swingen,and Jianyi Zhang. 2013. Induced Pluripotent Stem Cells and Their Potential for Basic and Clinical Sciences. Curr Cardiol Rev. 2013 Feb; 9(1): 63–72. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3584308/.
- Mark F. Pittenger, Dennis E. Discher, Bruno M. Péault, Donald G. Phinney, Joshua M. Hare & Arnold I. Caplan. 2019. Mesenchymal stem cell perspective: cell biology to clinical progress. npj Regenerative Medicine volume 4, Article number: 22 (2019)
- Ji Yoon Lee and Seok-Ho Hong. 2019. Hematopoietic Stem Cells and Their Roles in Tissue Regeneration. Int J Stem Cells. 2020; 13(1): 1–12.
- Abdelkrim Hmadcha, Alejandro Martin-Montalvo, Benoit R. Gauthier, Bernat Soria and Vivian Capilla-Gonzalez. 2020. Therapeutic Potential of Mesenchymal Stem Cells for Cancer Therapy. Front. Bioeng. Biotechnol., 05 February 2020 Sec. Biomaterials Volume 8 - 2020





