
Japanese encephalitis virus or JEV is a debilitating mosquito-borne Flavivirus disease that belongs to the same genus as dengue, yellow fever, and West Nile viruses. The rise of global transportation, trade, and climate change allow insects to easily carry disease thus, infecting animals as well as humans. Most JEV infections are endemic in tropical and subtropical regions. It later causes death when left untreated.
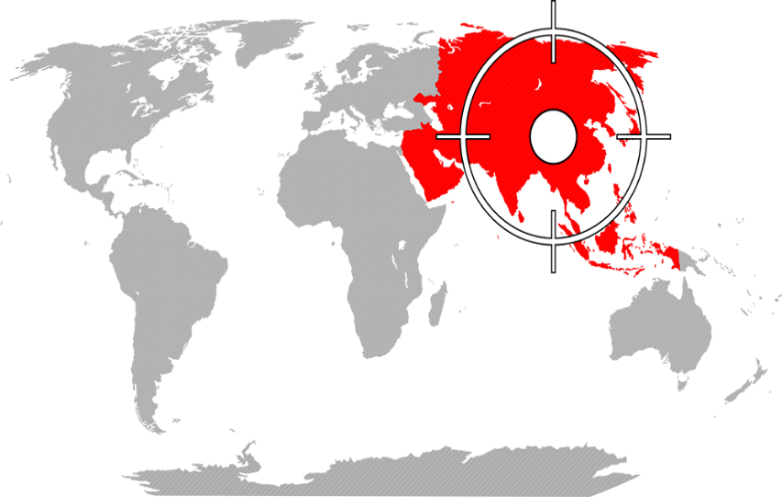
Figure 1. Hotspot countries for JEV Wave were highlighted in red.
JEV is transmitted to humans through bites from infected mosquitoes of the Culex species (mainly Culex tritaeniorhynchus). Travelers who go to rural areas in Asia and plan to stay for a long period of time are at higher risk of getting the disease. In mild climates such as in Northern Asia, the risk for JE is greater during summer and fall. In tropical and sub-tropical areas, the risk is all year-round.
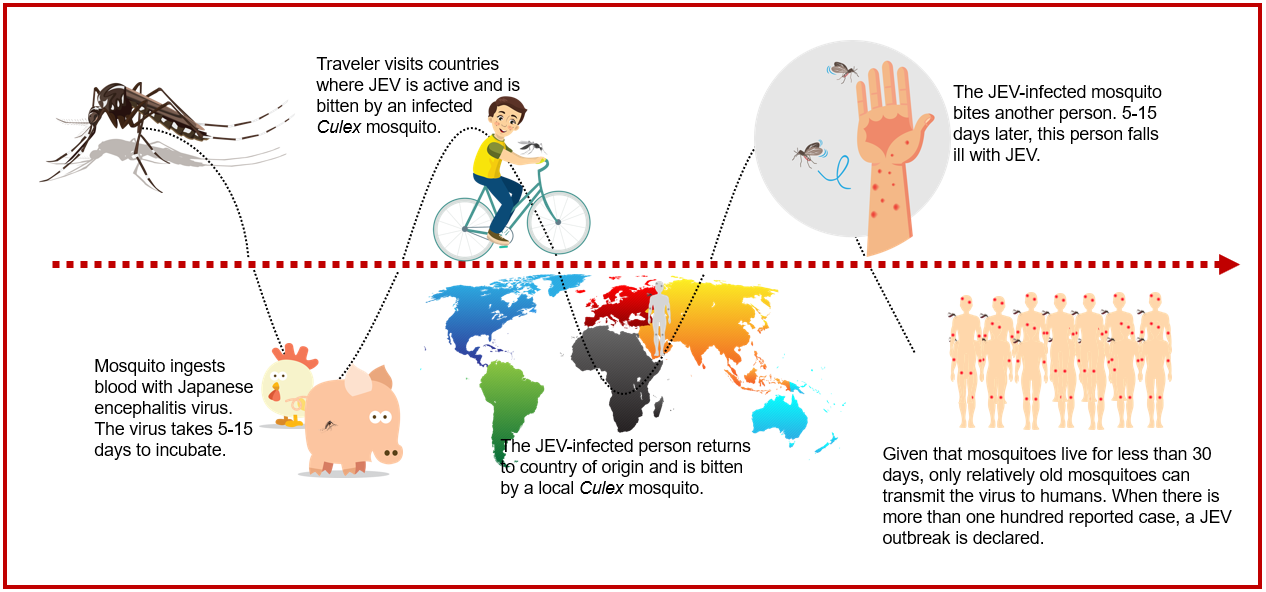
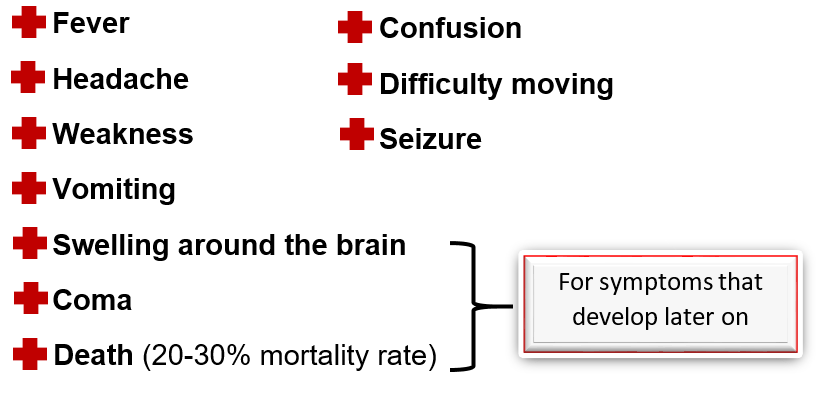
One bite is enough to infect a person. Symptoms take 5-15 days to appear
All travelers going to JE-endemic areas should take precautions to avoid mosquito bites to reduce the risk of contracting JE. Personal preventive measures include the use of repellents, vaporizers, and coils while wearing proper clothing. Vaccination should also be considered when there is a suitable environment for JE virus transmission. Safe and effective JE vaccines are available to prevent this disease. Four main types of vaccines currently in use are:

The VERO cell line is one of the most satisfactory cell lines based on its stability and well-documented performance in quality and quantity of viral yield. Although inactivated mouse brain-derived vaccines are of use today, these are gradually replaced by live attenuated and inactivated cell-based vaccines. New inactivated cell-based vaccines are manufactured from VERO cells and are currently in use in several countries.
Figure 2. VERO cells stained with crystal violet dye as observed under a microscope.
VERO cells are adherent in nature and proliferated in vivo either in static, planar systems or 3-D configured systems.
Unlike 2D systems which renders small surface area for growth of VERO cells, 3D systems offer a larger surface area for growth resulting to a higher product yield at the end of the culture production. BioNOC™ II is a 3D macroporous matrix, made of 100% PET that allows growth of VERO cells to 5x109 cells (Fig.2) with just 5.5 grams.
BioNOC II serves as the packed-bed of Tide Motion bioreactors. These bioreactors utilize the Tide Motion principle that is comparable to the cyclical high and low rise of the bodies of water on earth. In a culture system, this serves as the gentle upward and downward motion of the culture medium for aeration and nutrition exchange.
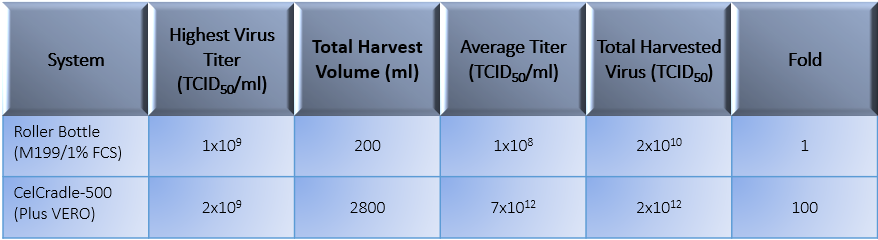
High viral titers should be considered when culturing VERO for JEV vaccine. Aside from the surface area of the carriers, Plus VERO is a component-defined cell culture medium that is animal- and human- component free, designed specifically for the growth of VERO cell line and suitable for growing viruses at a high yield. This culture medium also eliminates the need for serum as this component often leads to cell biological perspective concerns and ethical and animal welfare issues.
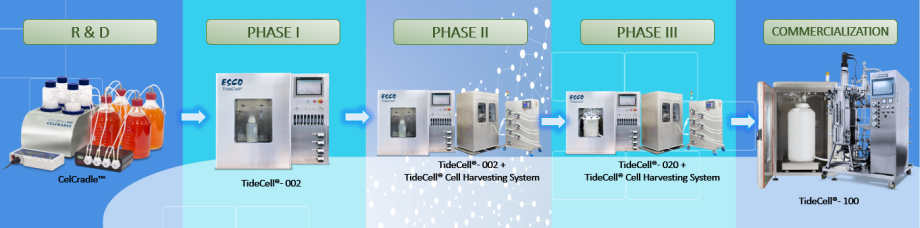
Esco VacciXcell Tide Motion bioreactors are linearly scalable from research and development phase to commercialization. See the whole process development below.

References:
Sign up to our newsletter and receive the latest news and updates about our products!
