
In early 2020, several companies have worked round-the-clock to commercialize the first COVID-19 vaccine. Pfizer/BioNTech, Sinovac, Moderna, Astrazeneca/Oxford, and Gamaleya emerged as the leading companies to develop the most widely used and distributed COVID-19 vaccines to date. These vaccines have shown promising results in controlled clinical trials, paving the way for their approval and emergency use authorizations. Their performance in the real world, or vaccine effectiveness, remains to be determined as mass vaccination programs kick off in the next few months.
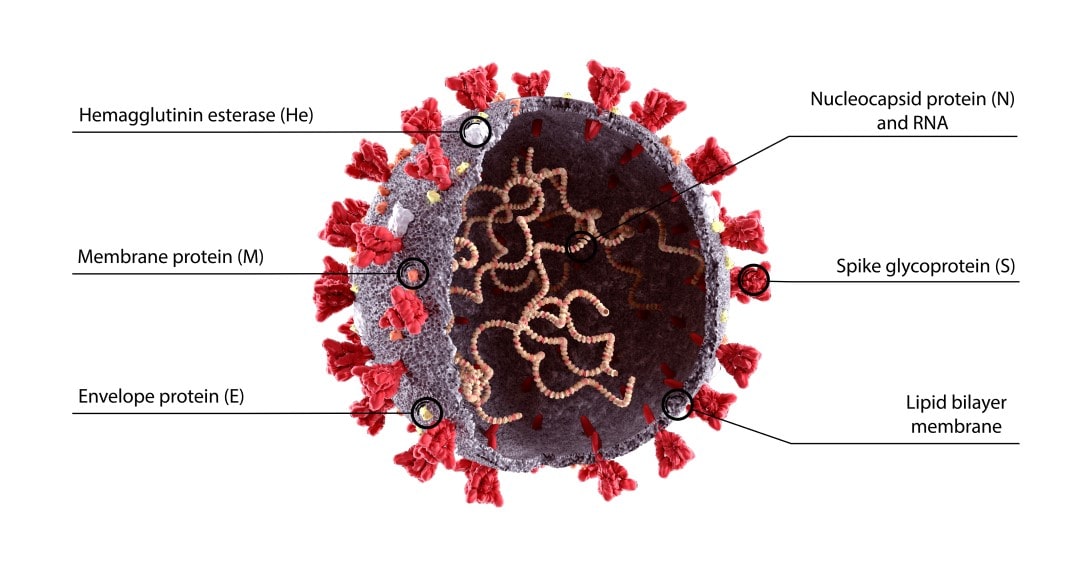
The designs of the leading vaccines in the market today are based on the early circulating strains of the SARS-CoV-2. The spike protein of the virus is a prominent target to design against as it is used for viral entry to the host cells, and is found abundantly on the viral surface which can be easily accessed by antibodies.
However, variants have emerged and have been detected late 2020 to early 2021, and have shown to reduce vaccine effectiveness, e.g., Oxford/Astrazeneca vaccine offers little to no protection against the South African B.1.351 variant. A study conducted by University of Oxford researchers shows some evidence that one of the mutations of this variant in the spike protein, E484K, may affect the neutralization of generated polyclonal and monoclonal antibodies. Recently, the surge of infection in India is fueled by the B.1.617 double variant (carrying features from California and South African variants). However, a peer-reviewed study by Indian scientists reveals that the most commonly used vaccine in their country protects against this double mutant variant.
The faulty replication machinery of the SARS-CoV-2 virus generates an estimated (from both theoretical and empirical mutation rate) 3 mutations per month for a specific lineage of virions infecting from host-to-host. Within a single host, the estimated mutation is 0.5 per infection, which can span most single base mutations. Variants today accumulated about 20-30 mutations, the B.1.1.7 UK variant having 40 mutations. This rate of mutation indicates the possibility of new variants to emerge persistently which can be dominant and can infect more people.
On the other hand, it is estimated that the current vaccination efforts would lead to only 10% of the world population being vaccinated by the end of this year. A model shows that to achieve herd immunity, 55% coverage is needed with a 90% vaccine efficiency and some social distancing measures. At the current rate the world is going and how fast variants are emerging, key stakeholders should ramp up monitoring and vaccination.
Countries should also continue to bolster their efforts to provide access for all to vaccination, as well as efforts to educate on the vaccination benefits. Low and middle-income countries would need equitable access to vaccines. Leading vaccine providers are also updating their vaccines to protect against emerging variants; some will provide booster shots for a third jab. Open technology sharing is being pressed by various groups to pharmaceutical and biotech companies in order to provide information for manufacturers to easily manufacture updated vaccines. Monitoring vaccine effectiveness and investigating breakthrough cases (or fully vaccinated individuals getting the disease) are of importance. Not only do we need to control human transmission, but as SARS-CoV-2 has been detected in minks in Denmark and infected humans, there is also a need to develop COVID-19 vaccines to protect animal reservoirs.
This pandemic has definitely challenged sectors and human ingenuity to develop and market technologies at a pace never seen before. It is a race against a replication machinery capable of spewing out potential infectious variants, in which we should provide these technologies to all so we leave no population where this virus can freely mutate. We can win this race against time, and we win by running together.
Sign up to our newsletter and receive the latest news and updates about our products!
